How Healthcare Became Sickcare
Authored by Charles Hugh Smith via OfTwoMinds blog,
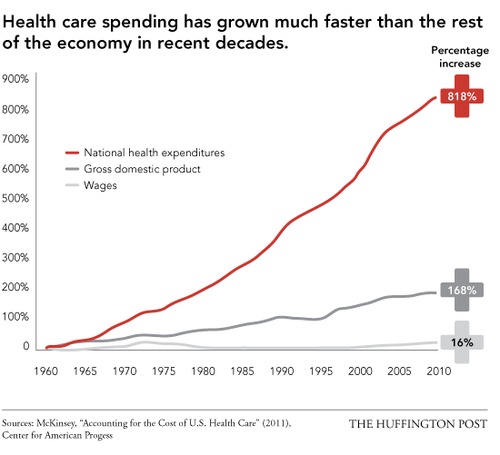
The financialization of healthcare started two generations ago and is now in a run-to-fail feedback loop of insolvency.
Long-time readers know I have been critical of U.S. healthcare for over a decade. When I use the term sickcare this is not a reflection on the hard work of frontline caregivers–it is a reflection of the financialization incentives that have distorted the system’s priorities and put it on a path to insolvency.
To describe how Healthcare became Sickcare, I’m sharing the perspective of an Insider. The financialization of healthcare started two generations ago and is now in a run-to-fail feedback loop of insolvency. As I have often said, Sickcare will bankrupt the nation all by itself. Here is the Insider’s essay:
* * *
As your readers try to make sense of the American health system and its response to COVID, they may benefit from a brief summary of the system’s current business model from someone on the inside.
It’s my hope that it will help them make sense of what is going on around them.
I read, see, and hear others inside the system scared for their livelihoods if they speak out and I’m ashamed of myself, as my livelihood no longer depends on my silence.
So I’m sharing this to speak for those who can’t.
For reasons beyond the scope of this study, and aside from a (very) few service lines, the delivery of healthcare is a low margin affair. Unless one keeps their overhead very low, profit is difficult to achieve.
Yet, the consolidated health systems which increasingly dominate the landscape are clearly high-overhead concerns, what with their staggering management bandwidth, gleaming palaces of healing, and obscene executive compensation.
How does one square this?
Health systems generate revenue from:
1. A (very) small number of profitable service lines, mostly plastics, some ortho, and a smattering of others.
2. Inflated book value of their commercial real estate, often untaxed due to religious/not-for-profit status.
3. Bulk and individual resale of patient information.
4. Kickbacks from suppliers, legal (purchase rebates) and illegal (direct payments).
5. Government grants.
Health systems don’t make their money from the delivery of healthcare, they make their money by charging for the redirection of the firehose of third-party payments to which the delivery of healthcare grants them access. This is true for any health system which exceeds a certain fairly modest size and provides the majority of their care through third-party payers such as Medicare.
It is true regardless of their IRS designation; for-profit, not-for-profit, religious. The religious sponsored ones use their status as a religion to put themselves, politically and legally, at the greatest possible distance from IRS scrutiny.
Under this model, the organization’s goal is simply to keep up the facade of delivering healthcare at the lowest possible cost and generate maximum revenue from all the secondary effects.
Thank you Accountable Care Act.
For example, health systems:
1. Allegedly collude with each other to keep clinicians and nurses wages as low as possible
2. Ensure, if not favorable, at least neutral media coverage through
a. The presence of media company leadership on their boards and vise-versa
b. Direct payment to those organizations either through overpriced advertising or direct payoffs to their executives.
3. Emphasize the few profit-generating service lines, most recently COVID. Two years into the pandemic and for no real reason, COVID diagnoses still carry bonus compensation to the health systems. The use of certain COVID-related meds carry “rebate” payments back to the systems.
4. reduce supply costs by either
a. Purchasing the vendors directly
b. Utilizing the most inexpensive supply chains whose quality is just enough to maintain the facade.
This last tactic is why there was such a huge shortage of PPE at the beginning of the pandemic. Supply chains reached into China where the least expensive options were found. Unfortunately, those supply chains were fragile and dependence on them left few domestic suppliers able to ramp up deliveries.
This is also why there is such a large number of “financializers” in executive positions. Their passion isn’t healthcare, it’s the access to the 20% of GDP the industry grants them. When the pandemic hit, how many CEOs did you see in working in the ER for an hour or so a week to demonstrate solidarity with the minimum wage employees who, at unknown risk to themselves, were keeping the place running?
None. They were all in the second homes in Florida. Their hearts are in finance, not healthcare.
This worldview explains so many puzzling things.
Q. Why are poor conditions at hospitals not being reported?
A. Collusion with the media
Q. Why are hospitals able to let go of so many employees, even in the middle of a pandemic?
A. They only need enough to service their few profitable lines (COVID) while keeping up the appearance of delivering healthcare.
Q. Why is the capacity for the few profit-generating service lines, such as COVID ICU care, growing while it’s so difficult to get an appointment for more mundane services?
A. That’s where the money is.
Q. Why are clinicians and nurses changing careers at an unprecedented rate?
A. The current business model is incompatible with their personal mission of service. Guffaw if you like. Yes, they too like to make money, but unlike the financial folks they must have an aspect of service in their vocation to be content. Otherwise, they also would have just gone into business. They are unable to square their personal mission with the commoditization of human life they are seeing.
So they leave.
Q. Why is the physician suicide rate now the highest among individuals with > 4 years college. At current growth rates, soon 1/10000 doctors will kill themselves every year, a phenomenal number.
A. See above, then add debt and disillusionment.
Consider this one of the fruits of delivering a subtle, subjective service such as healthcare through an assembly-line industrial model focused on making a buck. The line workers and their training are mismatched to the task. Force petroleum wild-catters to sell Mary Kay and you’ll get the same thing.
Q. Why do health systems continue to invest in commercial real estate?
A. They use pre-pandemic foot traffic numbers to boost both the valuations and the rental rates to tenants. Like in 2009, nobody has an interest in marking the value of their investments to market.
Q. Why does everyone in healthcare spend so much time on the computer?
A. Because the data they’re collecting is a significant source of revenue.
Q. Why does getting healthcare feel like such an assembly line?
A. Because that’s how the executives have been trained to keep down costs. They don’t care about individual patients, they care about “patients” in aggregate for the reasons outlined above.
Q. Why are health systems so dead set on getting their employees the COVID shot?
A. “Rebates” from the supplier and ingratiating themselves to the political and regulatory classes who themselves are getting kickbacks as well.
Q. Why are health systems emphasizing telemedicine?
A. Because they believe they can squeeze more productivity out of their providers while paying them the same– it’s a tactic to decrease the costs associated with keeping up the facade of delivering healthcare.
Is your health system one of these? The better their customer service, the less likely your health system follows this model.
This of course is an extension of Gresham’s Law; Bad Chases Out Good, money first, then everything else. When the currency is fake, it corrodes society itself. It is the tsunami of valueless fiat that makes keeps the whole edifice erect. The percentage of GDP we “spend” on “healthcare” actually represents the percent of GDP that’s skimmed using healthcare as a grift.
I think about the reader who operates under the assumption that health systems are in the business of delivering healthcare.
They are actually in the business of, well, business.
And they’ve used their position to prevent any competition at scale. Fortunately, you and I don’t need healthcare at scale, we just need healthcare. So, look for a clinician who takes cash. Go to DPcare.org or check out the Surgery Center of Oklahoma City. Cleveland Clinic will do your bypass for a flat fee, and pay for any complications. The prices are much less than one would expect, and you get great access to your personal clinician, not as one of 5000 patients, but as one of 500.
We must relieve ourselves of the idea that our Medicare and health insurance premiums pay for healthcare. They’re just taxes for which we’ll gain limited value, at best they represent catastrophic coverage. To get valuable healthcare, we are going to have to pay for it ourselves.
I don’t represent, personally provide, or have any financial interest in cash-pay healthcare.
As resources decline and health systems focus increasingly on the grift rather than care, direct payment for healthcare will continue to grow under the radar–as it doesn’t (yet) threaten the health systems’ position.
Compared to expectations, cash-pay is surprisingly inexpensive, the care experience is better, and it includes very little valueless, harmful, or excess care.
It is my hope that the worldview above helps your readers explain and possibly predict the behavior of these health systems going forward.
* * *
Thank you, Insider. As I have have noted many times, if you still believe that America’s system is “the finest in the world” and is endlessly sustainable, please study these three charts and extend the trendlines.
* * *
My new book is now available at a 10% discount this month: Global Crisis, National Renewal: A (Revolutionary) Grand Strategy for the United States (Kindle $8.95, print $20). If you found value in this content, please join me in seeking solutions by becoming a $1/month patron of my work via patreon.com.
Tyler Durden
Sun, 03/20/2022 – 11:30
Recent Comments